Oxygen for premature babies – important for survival, but with consequences for the lung function of children
It is a kind of vicious circle in neonatology, neonatal medicine:
Because the lungs of premature babies are not yet mature enough, the so-called respiratory distress syndrome develops and the babies cannot breathe on their own. The “preemies”, as parents and doctors affectionately call the youngest patients, must therefore be artificially ventilated. The use of oxygen therapy, however, leads to a chronic lung disease, bronchopulmonary dysplasia (BPD). BPD makes children susceptible to other respiratory diseases and limits their lung function. Using the AIRR study data, the team led by Dr. Anne Hilgendorff wants to find out whether and how this "vicious circle" can be broken:
"We want to better understand and make an earlier diagnosis of the lung condition of babies born prematurely, called BPD, so that in the future we can already say in the delivery room: We are now better able to help your child and avoid long-term complications."
PD Dr. Anne Hilgendorff
Bronchopulmonary dysplasia: Detect earlier, treat better
The problem with preterm babies and BPD: So far, it is only possible to diagnose very late which baby develops the lung disease and which baby does not. There is also a lack of understanding of the molecular mechanisms underlying BPD:
What impedes alveolar and capillary development in the lungs of premature infants? And how can we detect these damages as early as possible?
BPD is currently diagnosed shortly before release from the hospital, before the calculated date of birth is reached. A point in time at which many therapeutic opportunities are missed. One of the aims of the AIRR study: identify biomarkers in order to diagnose this chronic lung disease better and earlier.

© Helmholtz München
BPD on the track - innovative approaches in the search for biomarkers
Lung and lung tissue examinations as performed in various adult diseases are not possible in premature babies. The AIRR study team therefore uses three other modern approaches in its examination methods:
- Imaging Techniques (Magnetic Resonance Imaging, MRI)
- Pulmonary function tests
- Analysis of biosamples (pulmonary secretions, urine, blood)
By analyzing blood plasma, the AIRR team has already shown: There are three specific proteins as marker proteins that point to bronchopulmonary dysplasia. New strategies in magnetic resonance imaging led to further findings:
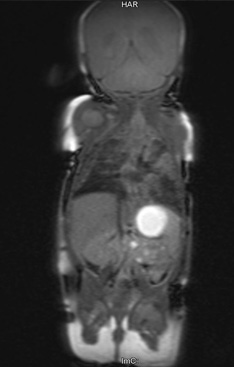
© LMU Clinic Munich
Evidence of BPD in MRI images
Dr. Kai Förster from Anne Hilgendorff's working group and experts of the Radiology Department at Munich University Hospital examined around 60 neonates with MRI. They looked at the proton density in the tissue, more precisely: how the atoms reorient themselves after irradiation. The subsequent statistical evaluation of the imaging data was done in collaboration with the Institute for Computational Biology (ICB) at the Helmholtz Zentrum.
The evaluation revealed: how long this reorientation of the atoms in the tissue lasts indicates the presence of Bronchopulmonary Dysplasia.
“Our results mark an important step towards improving image-based phenotyping of infants who are at risk or have developed the disease,” comments Dr. Hilgendorff. It is important, she stresses, that large perinatal centers now use this method and evaluate it jointly aiming at identifying potential subtypes of Bronchopulmonary Dysplasia.


